Glaucoma and myopia: risk factors, pathophysiology, and treatment
DOI:
https://doi.org/10.58931/cect.2022.1110Abstract
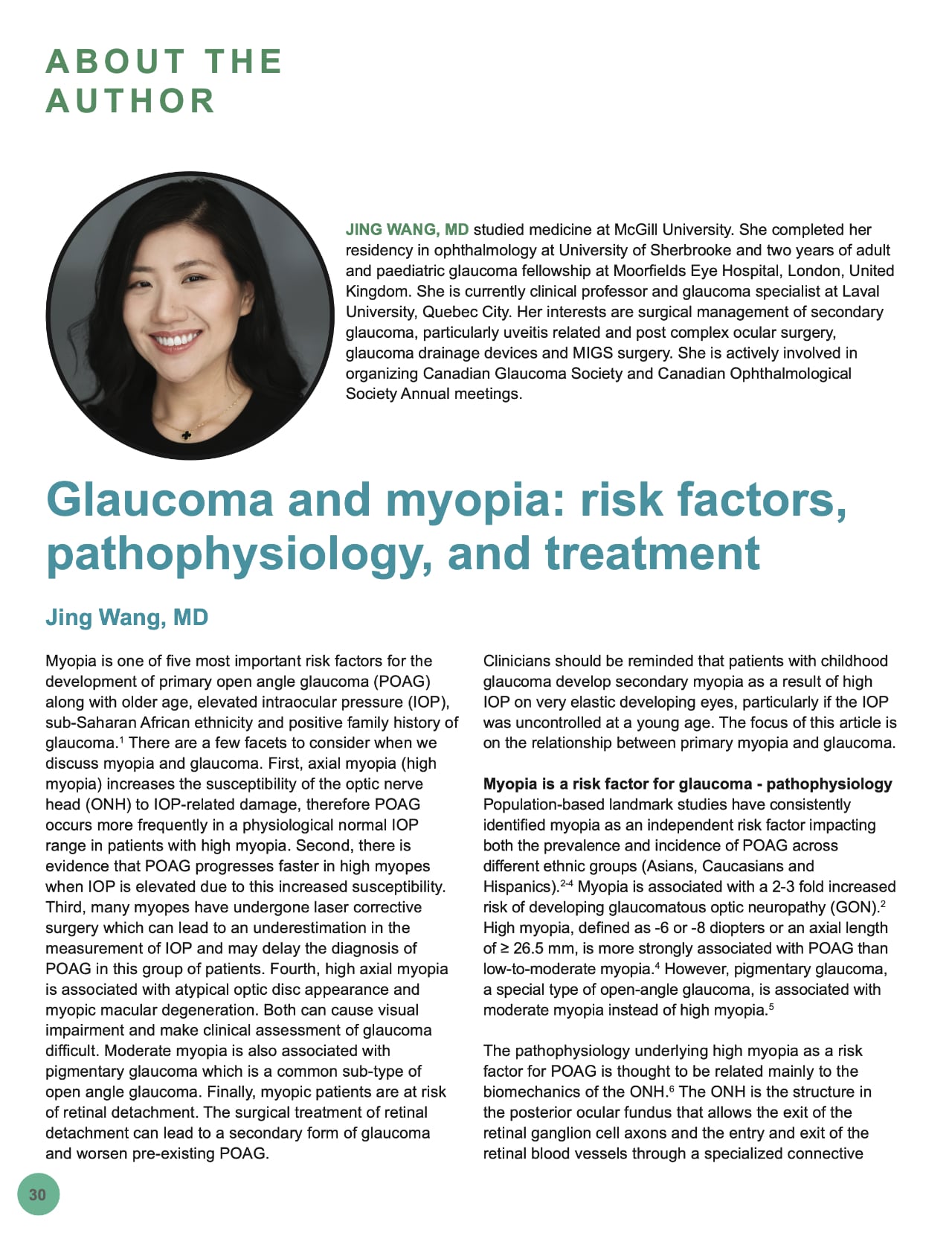
Myopia is one of five most important risk factors for the development of primary open angle glaucoma (POAG) along with older age, elevated intraocular pressure (IOP), sub-Saharan African ethnicity and positive family history of glaucoma. There are a few facets to consider when we discuss myopia and glaucoma. First, axial myopia (high myopia) increases the susceptibility of the optic nerve head (ONH) to IOP-related damage, therefore POAG occurs more frequently in a physiological normal IOP range in patients with high myopia. Second, there is evidence that POAG progresses faster in high myopes when IOP is elevated due to this increased susceptibility. Third, many myopes have undergone laser corrective surgery which can lead to an underestimation in the measurement of IOP and may delay the diagnosis of POAG in this group of patients. Fourth, high axial myopia is associated with atypical optic disc appearance and myopic macular degeneration. Both can cause visual impairment and make clinical assessment of glaucoma difficult. Moderate myopia is also associated with pigmentary glaucoma which is a common sub-type of open angle glaucoma. Finally, myopic patients are at risk of retinal detachment. The surgical treatment of retinal detachment can lead to a secondary form of glaucoma and worsen pre-existing POAG.
Clinicians should be reminded that patients with childhood glaucoma develop secondary myopia as a result of high IOP on very elastic developing eyes, particularly if the IOP was uncontrolled at a young age. The focus of this article is on the relationship between primary myopia and glaucoma.
References
Jonas JB, Aung T, Bourne RR, Bron AM, Ritch R, Panda-Jonas S. Glaucoma. Lancet (London, England). 2017; 390(10108): 2183-2193. doi:10.1016/S0140-6736(17)31469-1 DOI: https://doi.org/10.1016/S0140-6736(17)31469-1
Mitchell P, Hourihan F, Sandbach J, Wang JJ. The relationship between glaucoma and myopia: the Blue Mountains Eye Study. Ophthalmology. 1999; 106(10): 2010-2015. doi:10.1016/s0161-6420(99)90416-5 DOI: https://doi.org/10.1016/S0161-6420(99)90416-5
Kuzin AA, Varma R, Reddy HS, Torres M, Azen SP, Los Angeles Latino Eye Study Group. Ocular biometry and open-angle glaucoma: the Los Angeles Latino Eye Study. Ophthalmology. 2010; 117(9): 1713-1719. doi:10.1016/j.ophtha.2010.01.035 DOI: https://doi.org/10.1016/j.ophtha.2010.01.035
Xu L, Wang Y, Wang S, Wang Y, Jonas JB. High myopia and glaucoma susceptibility the Beijing Eye Study. Ophthalmology. 2007; 114(2): 216-220. doi:10.1016/j.ophtha.2006.06.050 DOI: https://doi.org/10.1016/j.ophtha.2006.06.050
Richter CU, Richardson TM, Grant WM. Pigmentary dispersion syndrome and pigmentary glaucoma. A prospective study of the natural history. Arch Ophthalmol (Chicago, Ill 1960). 1986; 104(2): 211-215. doi:10.1001/archopht.1986.01050140065021 DOI: https://doi.org/10.1001/archopht.1986.01050140065021
Jonas JB, Wang YX, Dong L, Panda-Jonas S. High Myopia and Glaucoma-Like Optic Neuropathy. Asia-Pacific J Ophthalmol (Philadelphia, Pa). 9(3): 234-238. doi:10.1097/APO.0000000000000288 DOI: https://doi.org/10.1097/APO.0000000000000288
Mayama C, Suzuki Y, Araie M, et al. Myopia and advanced-stage open-angle glaucoma. Ophthalmology. 2002; 109(11): 2072-2077. doi:10.1016/s0161-6420(02)01175-2 DOI: https://doi.org/10.1016/S0161-6420(02)01175-2
Jonas JB, Nagaoka N, Fang YX, Weber P, Ohno-Matsui K. Intraocular Pressure and Glaucomatous Optic Neuropathy in High Myopia. Invest Ophthalmol Vis Sci. 2017; 58(13): 5897-5906. doi:10.1167/iovs.17-21942 DOI: https://doi.org/10.1167/iovs.17-21942
Pepose JS, Feigenbaum SK, Qazi MA, Sanderson JP, Roberts CJ. Changes in corneal biomechanics and intraocular pressure following LASIK using static, dynamic, and noncontact tonometry. Am J Ophthalmol. 2007; 143(1): 39-47. doi:10.1016/j.ajo.2006.09.036 DOI: https://doi.org/10.1016/j.ajo.2006.09.036
Wang YX, Panda-Jonas S, Jonas JB. Optic nerve head anatomy in myopia and glaucoma, including parapapillary zones alpha, beta, gamma and delta: Histology and clinical features. Prog Retin Eye Res. 2021; 83:100933. doi:10.1016/j.preteyeres.2020.100933 DOI: https://doi.org/10.1016/j.preteyeres.2020.100933
Tan NYQ, Sng CCA, Jonas JB, Wong TY, Jansonius NM, Ang M. Glaucoma in myopia: diagnostic dilemmas. Br J Ophthalmol. 2019; 103(10): 1347-1355. doi:10.1136/bjophthalmol-2018-313530 DOI: https://doi.org/10.1136/bjophthalmol-2018-313530
Leung CK-S, Yu M, Weinreb RN, et al. Retinal nerve fiber layer imaging with spectral-domain optical coherence tomography: interpreting the RNFL maps in healthy myopic eyes. Invest Ophthalmol Vis Sci. 2012; 53(11): 7194-7200. doi:10.1167/iovs.12-9726 DOI: https://doi.org/10.1167/iovs.12-9726
Kim KE, Jeoung JW, Park KH, Kim DM, Kim SH. Diagnostic classification of macular ganglion cell and retinal nerve fiber layer analysis: differentiation of false-positives from glaucoma. Ophthalmology. 2015; 122(3): 502-510. doi:10.1016/j.ophtha.2014.09.031 DOI: https://doi.org/10.1016/j.ophtha.2014.09.031
Doshi A, Kreidl KO, Lombardi L, Sakamoto DK, Singh K. Nonprogressive Glaucomatous Cupping and Visual Field Abnormalities in Young Chinese Males. Ophthalmology. 2007; 114(3): 472-479. doi:10.1016/j.ophtha.2006.07.036 DOI: https://doi.org/10.1016/j.ophtha.2006.07.036
Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet (London, England). 2019; 393(10180): 1505-1516. doi:10.1016/S0140-6736(18)32213-X DOI: https://doi.org/10.1016/S0140-6736(18)32213-X
Scott A, Kotecha A, Bunce C, et al. YAG laser peripheral iridotomy for the prevention of pigment dispersion glaucoma a prospective, randomized, controlled trial. Ophthalmology. 2011; 118(3): 468-473. doi:10.1016/j.ophtha.2010.07.026 DOI: https://doi.org/10.1016/j.ophtha.2010.07.026
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Canadian Eye Care Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.