The evolving role of OCT in pathologic myopia
DOI:
https://doi.org/10.58931/cect.2022.115Abstract
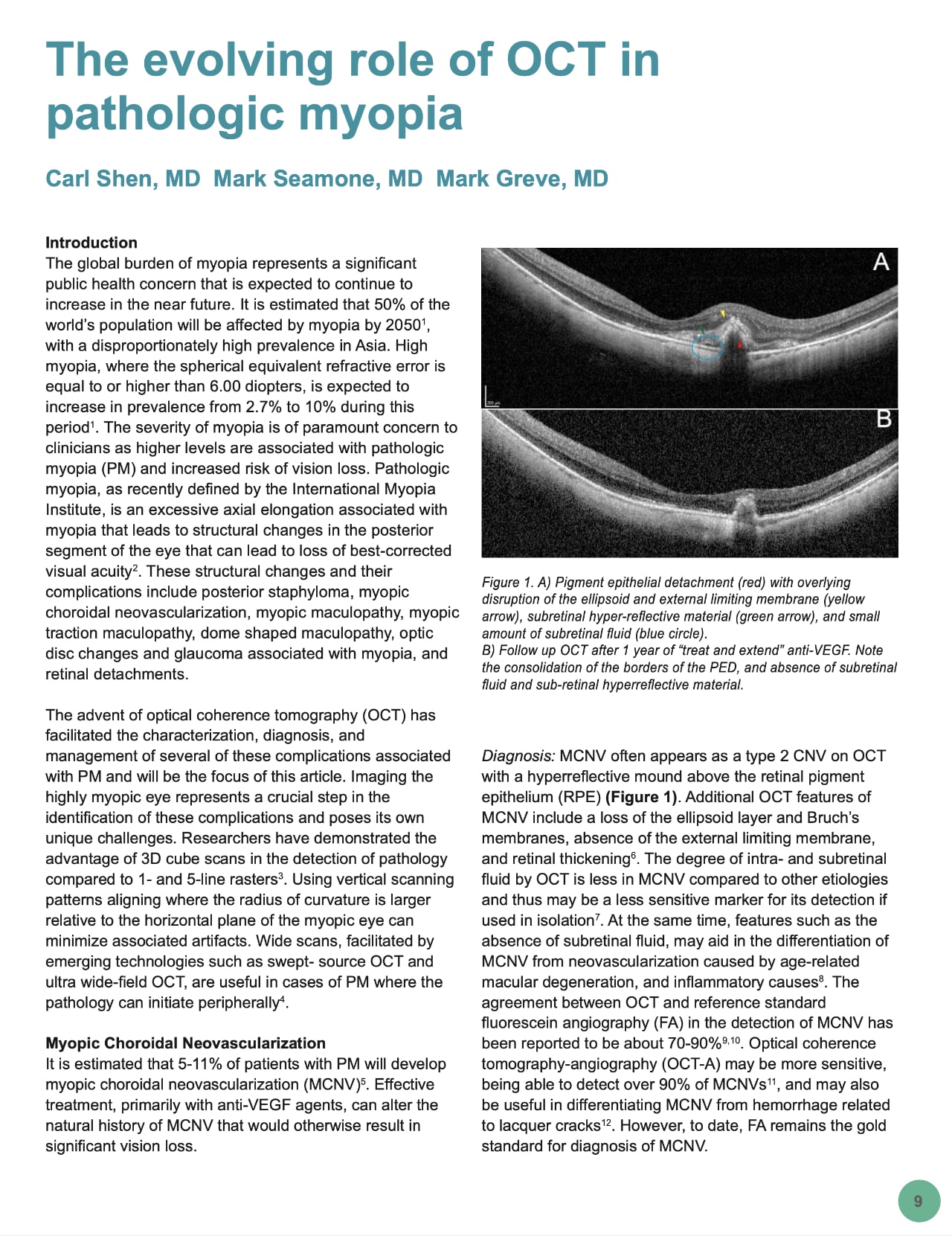
The global burden of myopia represents a significant public health concern that is expected to continue to increase in the near future. It is estimated that 50% of the world’s population will be affected by myopia by 2050, with a disproportionately high prevalence in Asia. High myopia, where the spherical equivalent refractive error is equal to or higher than 6.00 diopters, is expected to increase in prevalence from 2.7% to 10% during this period. The severity of myopia is of paramount concern to clinicians as higher levels are associated with pathologic myopia (PM) and increased risk of vision loss. Pathologic myopia, as recently defined by the International Myopia Institute, is an excessive axial elongation associated with myopia that leads to structural changes in the posterior segment of the eye that can lead to loss of best-corrected visual acuity. These structural changes and their complications include posterior staphyloma, myopic choroidal neovascularization, myopic maculopathy, myopic traction maculopathy, dome shaped maculopathy, optic disc changes and glaucoma associated with myopia, and retinal detachments.
The advent of optical coherence tomography (OCT) has facilitated the characterization, diagnosis, and management of several of these complications associated with PM and will be the focus of this article. Imaging the highly myopic eye represents a crucial step in the identification of these complications and poses its own unique challenges. Researchers have demonstrated the advantage of 3D cube scans in the detection of pathology compared to 1- and 5-line rasters. Using vertical scanning patterns aligning where the radius of curvature is larger relative to the horizontal plane of the myopic eye can minimize associated artifacts. Wide scans, facilitated by emerging technologies such as swept- source OCT and ultra wide-field OCT, are useful in cases of PM where the pathology can initiate peripherally.
References
Holden BA, Fricke TR, Wilson DA, et al. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-1042. DOI: https://doi.org/10.1016/j.ophtha.2016.01.006
Flitcroft DI, He M, Jonas JB, et al. IMI – Defining and Classifying Myopia: A Proposed Set of Standards for Clinical and Epidemiologic Studies. Invest Ophthalmol Vis Sci. 2019;60(3):M20-M30. DOI: https://doi.org/10.1167/iovs.18-25957
Sayanagi K, Morimoto Y, Ikuno Y, Tano Y. Spectral-domain optical coherence tomographic findings in myopic foveoschisis. Retina. 2010;30(4):623-628. DOI: https://doi.org/10.1097/IAE.0b013e3181ca4e7c
Ohno-Matsui K, Fang Y, Shinohara K, Takahashi H, Uramoto K, Yokoi T. Imaging of Pathologic Myopia. Asia-Pacific J Ophthalmol (Philadelphia, Pa). 2019;8(2):172-177.
Wong TY, Ferreira A, Hughes R, Carter G, Mitchell P. Epidemiology and disease burden of pathologic myopia and myopic choroidal neovascularization: an evidence-based systematic review. Am J Ophthalmol. 2014;157(1). DOI: https://doi.org/10.1016/j.ajo.2013.08.010
Milani P, Pece A, Pierro L, Bergamini F. Imaging of naive myopic choroidal neovascularization by spectral-domain optical coherence tomography. Ophthalmologica. 2014;232(1):28-36. DOI: https://doi.org/10.1159/000357980
Lai TYY, Cheung CMG. Myopic Choroidal Neovascularization: Diagnosis and Treatment. Retina. 2016;36(9):1614-1621. DOI: https://doi.org/10.1097/IAE.0000000000001227
Zicarelli F, Azzolini C, Cornish E, et al. Optical coherence tomography features of choroidal neovascularization and their correlation with age, gender, and underlying disease. Retina. 2021;41(5):1076-1083. DOI: https://doi.org/10.1097/IAE.0000000000002984
Leveziel N, Caillaux V, Bastuji-Garin S, Zmuda M, Souied EH. Angiographic and optical coherence tomography characteristics of recent myopic choroidal neovascularization. Am J Ophthalmol. 2013;155(5):913- 919. DOI: https://doi.org/10.1016/j.ajo.2012.11.021
Iacono P, Giorno P, Varano M, Parravano M. Structural and optical coherence tomography angiography in myopic choroidal neovascularization: Agreement with conventional fluorescein angiography. Eur J Ophthalmol. 2021;31(1):149-157. DOI: https://doi.org/10.1177/1120672119882333
Miyata M, Ooto S, Hata M, et al. Detection of Myopic Choroidal Neovascularization Using Optical Coherence Tomography Angiography. Am J Ophthalmol. 2016;165:108-114. DOI: https://doi.org/10.1016/j.ajo.2016.03.009
Battista M, Sacconi R, Borrelli E, et al. Discerning Between Macular Hemorrhages Due to Macular Neovascularization or Due to Spontaneous Bruch’s Membrane Rupture in High Myopia: A Comparative Analysis Between OCTA and Fluorescein Angiography. Ophthalmol Ther. 2022;11(2):821-831. DOI: https://doi.org/10.1007/s40123-022-00484-0
Introini U, Casalino G, Querques G, Gimeno AT, Scotti F, Bandello F. Spectral-domain OCT in anti-VEGF treatment of myopic choroidal neovascularization. Eye (Lond). 2012;26(7):976-982. DOI: https://doi.org/10.1038/eye.2012.75
Bruyère E, Caillaux V, Cohen SY, et al. Spectral-Domain Optical Coherence Tomography of Subretinal Hyperreflective Exudation in Myopic Choroidal Neovascularization. Am J Ophthalmol. 2015;160(4):749-758.e1. DOI: https://doi.org/10.1016/j.ajo.2015.07.004
Ikuno Y, Jo Y, Hamasaki T, Tano Y. Ocular risk factors for choroidal neovascularization in pathologic myopia. Invest Ophthalmol Vis Sci. 2010;51(7):3721-3725. DOI: https://doi.org/10.1167/iovs.09-3493
Ahn SJ, Park KH, Woo SJ. Subfoveal Choroidal Thickness Changes Following Anti-Vascular Endothelial Growth Factor Therapy in Myopic Choroidal Neovascularization. Invest Ophthalmol Vis Sci. 2015;56(10):5794-5800. DOI: https://doi.org/10.1167/iovs.14-16006
Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol (Chicago, Ill 1960). 2004;122(10):1455-1460. DOI: https://doi.org/10.1001/archopht.122.10.1455
Parolini B, Palmieri M, Finzi A, et al. The new Myopic Traction Maculopathy Staging System. Eur J Ophthalmol. 2021;31(3):1299-1312. DOI: https://doi.org/10.1177/1120672120930590
Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013;156(5). DOI: https://doi.org/10.1016/j.ajo.2013.06.031
Ripandelli G, Rossi T, Scarinci F, Scassa C, Parisi V, Stirpe M. Macular vitreoretinal interface abnormalities in highly myopic eyes with posterior staphyloma: 5-year follow-up. Retina. 2012;32(8):1531-1538. DOI: https://doi.org/10.1097/IAE.0b013e318255062c
Jo Y, Ikuno Y, Nishida K. Retinoschisis: a predictive factor in vitrectomy for macular holes without retinal detachment in highly myopic eyes. Br J Ophthalmol. 2012;96(2):197-200. DOI: https://doi.org/10.1136/bjo.2011.203232
Sborgia G, Boscia F, Niro A, et al. Morphologic and functional outcomes of different optical coherence tomography patterns of myopic foveoschisis after vitrectomy and inner limiting membrane peeling. Eye (Lond). 2019;33(11):1768-1775. DOI: https://doi.org/10.1038/s41433-019-0490-3
Grewal PS, Lapere SRJ, Gupta RR, Greve M. Macular buckle without vitrectomy for myopic macular schisis: a Canadian case series. Can J Ophthalmol. 2019;54(1):60-64. DOI: https://doi.org/10.1016/j.jcjo.2018.02.014
Alkabes M, Mateo C. Macular buckle technique in myopic traction maculopathy: a 16-year review of the literature and a comparison with vitreous surgery. Graefes Arch Clin Exp Ophthalmol. 2018;256(5):863- 877. DOI: https://doi.org/10.1007/s00417-018-3947-3
Grewal PS, Seamone M, Greve M, Deveau A, Gupta RR. Internal Chandelier-Assisted Macular Buckling for Myopic Foveoschisis. Retin Cases Brief Rep. 2020;Publish Ah.
Bruyère E, Philippakis E, Dupas B, Nguyen-Kim P, Tadayoni R, Couturier A. Benefit of interoperative optical coherence tomography for vitreomacular surgery in highly myopic eyes. Retina. 2018;38(10):2035-2044. DOI: https://doi.org/10.1097/IAE.0000000000001827
Parolini B, Palmieri M, Finzi A, Frisina R. Proposal for the management of myopic traction maculopathy based on the new MTM staging system. Eur J Ophthalmol. 2021;31(6):3265-3276. DOI: https://doi.org/10.1177/1120672120980943
Ohno-Matsui K, Kawasaki R, Jonas JB, et al. International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015;159(5):877-883.e7. DOI: https://doi.org/10.1016/j.ajo.2015.01.022
Fang Y, Yokoi T, Nagaoka N, et al. Progression of Myopic Maculopathy during 18-Year Follow-up. Ophthalmology. 2018;125(6):863- 877. DOI: https://doi.org/10.1016/j.ophtha.2017.12.005
Fang Y, Du R, Nagaoka N, et al. OCT-Based Diagnostic Criteria for Different Stages of Myopic Maculopathy. Ophthalmology. 2019;126(7):1018-1032. DOI: https://doi.org/10.1016/j.ophtha.2019.01.012
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 Canadian Eye Care Today

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
